Lymphedema Treatment
Lymphedema is a chronic disease that occurs due to an abnormality or injury to the lymphatic system. When the lymphatic system is injured or abnormal, the lymph fluid cannot drain, and this protein-rich fluid accumulates in the interstitium, leading to debilitating swelling of the involved body part. The most common cause of lymphedema in the U.S. is after cancer treatment, where lymph nodes are removed as part of the treatment, leading to a blockage of the lymphatic flow.
How does lymphedema occur in breast cancer?
The lymphatic collectors of the arm drain in most patients through the lymph nodes of the axilla or armpit. The lymphatic collectors of the breast also drain into the same lymph nodes. In breast cancer treatment, the armpit nodes are sampled to determine if the cancer has spread beyond the breast. This is called a sentinel node biopsy.
Sometimes, if there is cancer in the sentinel lymph node, most of the armpit nodes have to be removed to prevent the cancer from coming back into the axilla (a procedure called an axillary lymph node dissection, or ALND). The risk of developing lymphedema after a sentinel lymph node biopsy is small, but it can still occur. The risk of developing lymphedema after most armpit nodes are removed is much greater, especially if the axilla is treated with postoperative radiation therapy. The risk of developing lymphedema in this situation is about 20 to 30%.
What are the risk factors for developing lymphedema in breast cancer?
- Removing the majority of the axillary lymph nodes (ALND)
- Removing more than six nodes when performing a sentinel lymph node biopsy
- Receiving radiation to the axilla
- Performing a mastectomy without reconstruction
- Having a BMI greater than 30
- Developing a postoperative infection
- Developing a postoperative hematoma (blood clot in the wound)
- Receiving Taxane therapy
What do I do if I develop lymphedema of the arm?
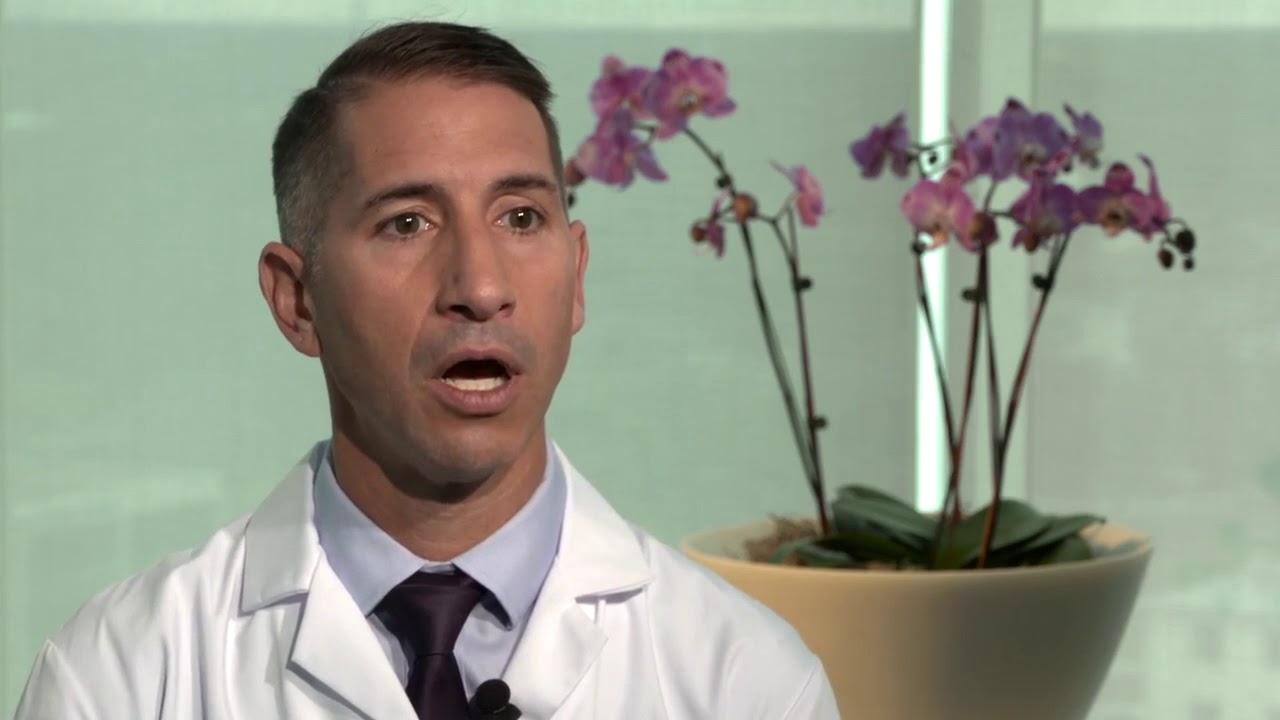
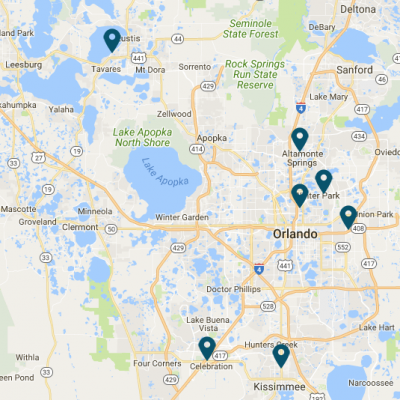
At AdventHealth, we have a surveillance program that will follow you closely after you have started your breast cancer treatment. We will measure your arm volumes over time and use bioimpedance to determine if you are developing an early form of lymphedema. If you do develop lymphedema, you’ll be referred to our lymphatic therapist, who will begin therapy immediately. Our therapists are located on multiple campuses for your convenience.
Therapy consists of performing Complete Decongestive Therapy (CDT), which includes the following:
- Manual lymphatic drainage – a form of light massage to remove lymph fluid from the affected arm
- External compression – usually a custom-fitted compression garment for the hand and arm that applies pressure on the skin and tissues to prevent the lymph fluid from reaccumulating.
- Exercise with compression encourages the flow of lymph fluid out of the arm as the muscle contracts against a compression garment.
- Skin care – this consists of using moisturizing lotion to keep the skin of the arm soft and supple and prevent cracks in the skin, which can lead to an infection (cellulitis)
What happens if I have lymphedema of the arm, and I don’t get it treated?
Once you develop lymphedema, the swelling will worsen over time unless it is controlled with CDT. Once significant swelling sets in the lymph fluid in the tissues, it causes inflammation of the interstitial space, leading to the accumulation of fat cells and scarring, which is referred to as lipo fibrosis. Once you develop this condition, it becomes very difficult to treat the involved arm. You are also at risk of developing serious infections of the arm called cellulitis that may require hospitalization for intravenous antibiotics.
Is there an operation that can help if I do develop lymphedema?
In our Center for Comprehensive Lymphatic Care (CCLC), we offer many surgical options for treating lymphedema.
Lympho-venous Bypass
One of the operations we perform is called a Lympho-Venous bypass in the axilla. This operation is performed before you develop lymphedema and is done at the time of the removal of the lymph nodes (ALND) during breast cancer treatment. In this operation, the lymphatic channels or collectors draining the arm are identified in the armpit using a variety of special dyes. Once the nodes are removed, these channels normally scar down, leading to lymph flow blockage and possible lymph fluid accumulation and lymphedema. Instead of allowing them to scar down, these collectors are sewn directly into an adjacent vein, allowing the lymph fluid to flow directly from the collectors into the vein. This operation significantly decreases the risk of developing lymphedema after an axillary lymph node dissection by approximately 50% but does not eliminate the risk.
Vascularized Lymph Node Transfer (VLNT)
If you develop lymphedema and are controlling your symptoms with CDT, we can improve the symptoms by performing a Vascularized Lymph Node Transfer. In this operation, four to six lymph nodes are removed from another part of your body and transferred to the armpit of the involved arm. The lymph node packet is attached to an artery and a vein in the armpit to provide nutrition and oxygen to the “transplanted” nodes. Once healing has occurred, the lymph nodes will begin forming new lymph channels that will help drain the excess lymph fluid accumulated in the involved arm. The use of custom compression garments is still necessary, albeit the duration of wear per day may be reduced.
Liposuction Debulking
Once you have developed more advanced lymphedema of the arm, the tissues swell not only due to the accumulation of lymph fluid but also due to the accumulation of fat cells and scar tissue. This lipo fibrosis causes the arm to enlarge further, and neither the VLNT nor LVB procedures will help reduce the arm volume. The only means of volume reduction is to remove the fat and scar layer with liposuction. This is often called lipo debulking or suction-assisted protein lipectomy (SAPL). This operation is usually performed six months after the VLNT procedure if necessary.